While deaths from Covid have proven most newsworthy, evidence is snowballing that Long Covid is also a serious issue, even affecting people in whom the disease initially appeared mild. Here, a few snippets from related articles and Twitter threads, links to these so may be of some use to anyone interested.
- You really don’t want long covid
- From mild symptoms to profound disability
- A systemic illness that has debilitated millions
- Long Covid risks lower with more healthy lifestyle factors
- Chance of long Covid increases with reinfections
- Disability to affect a generation
- Long Covid has multiple impacts in body
- Vaccines do not fully protect against long covid
- Brain fog among long covid symptoms
- Reduced blood flow to brain
- Higher risk of heart and pulmonary problems, and death
- Persistent hypertension – high blood pressure
- Signs of autoimmune disease in people with Long Covid
- Immune system damaged by Covid?
- Covid can cause diabetes
- Long Covid depleting workforces and potentially impacting economies
- Vitamin C and l-arginine may help
You really don’t want long covid
From mild symptoms to profound disability
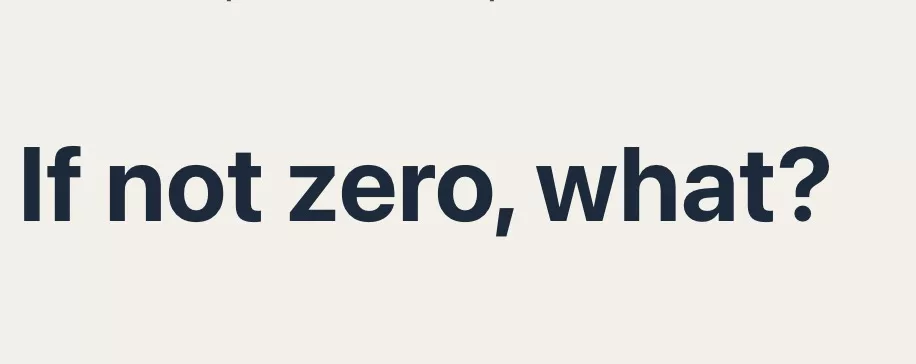
The disease burden spans from mild symptoms to profound disability, the scale making this a huge, new health-care challenge. Long COVID will likely be stratified into several more or less discrete entities with potentially distinct pathogenic pathways. The evolving symptom list is extensive, multi-organ, multisystem and relapsing–remitting, including fatigue, breathlessness, neurocognitive effects and dysautonomia. A range of radiological abnormalities in the olfactory bulb, brain, heart, lung and other sites have been observed in individuals with long COVID. Some body sites indicate the presence of microclots; these and other blood markers of hypercoagulation implicate a likely role of endothelial activation and clotting abnormalities. Diverse auto-antibody (AAB) specificities have been found, as yet without a clear consensus or correlation with symptom clusters. There is support for a role of persistent SARS-CoV-2 reservoirs and/or an effect of Epstein–Barr virus reactivation, and evidence from immune subset changes for broad immune perturbation.
The immunology of long COVID
A systemic illness that has debilitated millions
Long COVID is a multisystemic illness encompassing ME/CFS, dysautonomia, impacts on multiple organ systems, and vascular and clotting abnormalities. It has already debilitated millions of individuals worldwide, and that number is continuing to grow. On the basis of more than 2 years of research on long COVID and decades of research on conditions such as ME/CFS, a significant proportion of individuals with long COVID may have lifelong disabilities if no action is taken. Diagnostic and treatment options are currently insufficient, and many clinical trials are urgently needed to rigorously test treatments that address hypothesized underlying biological mechanisms, including viral persistence, neuroinflammation, excessive blood clotting and autoimmunity.
Long COVID: major findings, mechanisms and recommendations
Long Covid risks lower with more healthy lifestyle factors
In this prospective cohort study of 1981 women who reported a positive SARS-CoV-2 test from April 2020 to November 2021, adherence to a healthy lifestyle prior to infection was inversely associated with risk of PCC in a dose-dependent manner. Compared with those who did not have any healthy lifestyle factors, those with 5 or 6 had half the risk of PCC.
… Healthy lifestyle factors included healthy body mass index (BMI, 18.5-24.9; calculated as weight in kilograms divided by height in meters squared), never smoking, at least 150 minutes per week of moderate to vigorous physical activity, moderate alcohol intake (5 to 15 g/d), high diet quality (upper 40% of Alternate Healthy Eating Index–2010 score), and adequate sleep (7 to 9 h/d).
Adherence to Healthy Lifestyle Prior to Infection and Risk of Post–COVID-19 Condition
Chance of long Covid increases with reinfections
the study reported that long COVID diagnoses during the Omicron epoch occurred much closer to the index date of the infection or reinfection, and the number of long COVID diagnoses also showed an increase after reinfections with recent variants.
Study explores incidence, severity, and long COVID associations of SARS-CoV-2 reinfections
Disability to affect a generation
Long Covid could create a generation affected by disability, with people forced out of their homes and work, and some even driven to suicide, a leading expert has warned.
In an exclusive interview with the Guardian, Prof Danny Altmann – an immunologist at Imperial College London – said that the UK’s current approach to Covid fails to take the impact of infections sufficiently seriously, adding that more needs to be done to aid diagnosis and treatment of long Covid.
“It’s kind of an anathema to me that we’ve kind of thrown in the towel on control of Omicron wave infections and have said ‘it’s endemic, and we don’t care any more, because it’s very benign’,” he said. “It just isn’t. And there are new people joining the long Covid support groups all the time with their disabilities. It’s really not OK, and it’s heartbreaking.”
The Guardian: Long Covid could create a generation affected by disability, expert warns
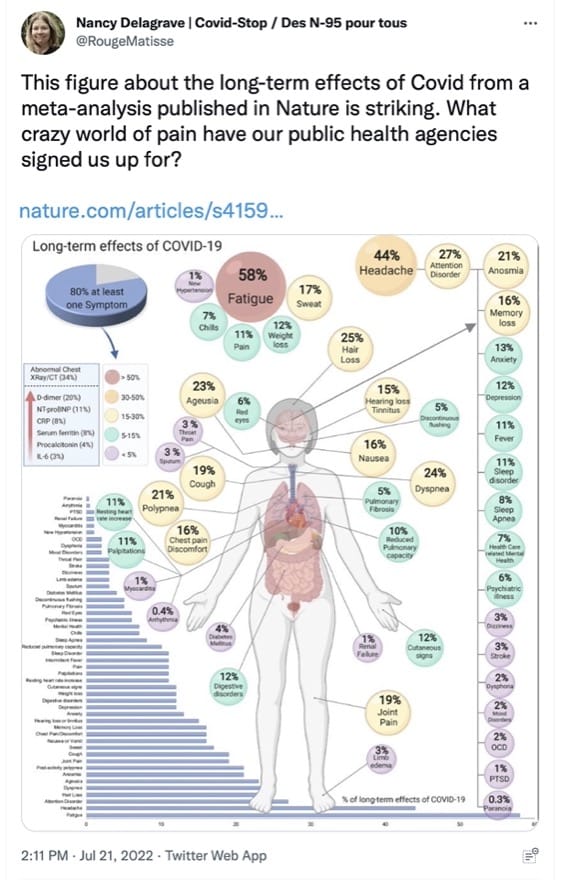
Long Covid has multiple impacts in body
Vaccines do not fully protect against long covid
Brain fog among long covid symptoms
How common are cognitive symptoms of long COVID? on Medical News Today includes:
As time goes on, [however,] there is more and more focus on the lingering effects of COVID-19, which experts refer to as long COVID.
For instance, there are reports of concentration and memory issues. A new study from the Universities of Cambridge and Exeter in the United Kingdom investigates just how common such problems are.
According to the study, 78% of people who reported they had long COVID symptoms during the study stated they experienced difficulties with concentration.
Also:
A large study comparing brain scans from the same individuals before and after SARS-CoV-2 infection suggests that brain changes could be a lingering outcome of even mild COVID-19. Writing in Nature, researchers at Oxford University’s Wellcome Centre for Integrative Neuroimaging reported that several months after study participants had SARS-CoV-2 infections, they had more gray matter loss and tissue abnormalities, mainly in the areas of the brain associated with smell, and more brain size shrinkage than participants who hadn’t been infected with the virus.
Even Mild COVID-19 May Change the Brain
Reduced blood flow to brain
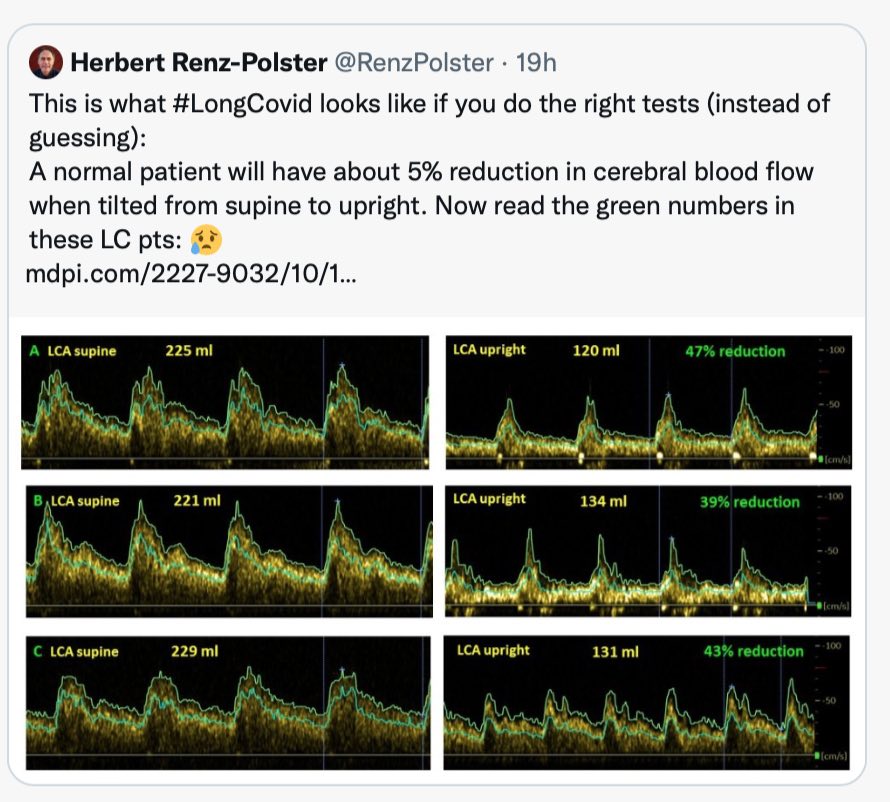
The paper linked to here has the clunky title Orthostatic Intolerance in Long-Haul COVID after SARS-CoV-2: A Case-Control Comparison with Post-EBV and Insidious-Onset Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patients
Higher risk of heart and pulmonary problems, and death
According to a new study published in JAMA Health Forum, people who caught COVID-19 in the past might be at higher risks of heart and pulmonary problems – and even a doubled risk of death.
…
It found that the group with long COVID had a higher mortality rate compared to the group without. Specifically, 2.8 per cent of individuals with long COVID had died compared to only 1.2 per cent of those who hadn’t caught the virus.The study further pinpoints fatigue, headache, and attention disorder as the most common symptoms experienced by people with long COVID.
“The biggest takeaway is that long COVID is a health condition that we need to continue to study and take seriously. We were particularly troubled by the elevated mortality risks for individuals with long COVID,” Dr Andrea DeVries, Staff Vice President for Health Services Research at Elevance Health and the lead author of the study, told Euronews Next.
Long COVID linked to higher mortality rates and long-term heart problems, new study finds
Persistent hypertension – high blood pressure
Incidence of new-onset persistent hypertension in patients with COVID-19 is higher than those with influenza, likely constituting a major health burden given the sheer number of patients with COVID-19.
Incidence of new-onset persistent hypertension in patients with COVID-19 is higher than those with influenza, likely constituting a major health burden given the sheer number of patients with COVID-19.
Signs of autoimmune disease in people with Long Covid
Blood samples drawn from patients with long COVID who are still suffering from fatigue and shortness of breath after a year show signs of autoimmune disease in those patients, according to a study published today in the European Respiratory Journal.
Autoimmune disease occurs when the immune system mistakenly attacks healthy parts of the body, instead of defending the body against disease. It causes conditions such as rheumatoid arthritis and lupus.
Long COVID patients show signs of autoimmune disease a year after infection
Two studies that use large cohorts now highlight that SARS-CoV-2 infection is linked to a substantially increased risk of developing a diverse spectrum of new-onset autoimmune diseases.
High risk of autoimmune diseases after COVID-19
Immune system damaged by Covid?
A person at the centre of the storm, sounding alarms about T cell “dysregulation” since the early days of the pandemic, has been a U.S. immunologist named Anthony Leonardi.
By dysregulation Leonardi means three effects of COVID:
- The hyperactivation of many T cells, which can prematurely age them
- The exuberant function of those hyperactivated T cells, which can then cause organ damage
- The exhaustion of those hyperactivated T cells, which implies they aren’t winning the battle against viral proteins they are supposed to defeat.
In other words, argues Leonardi, T cells are becoming hyperactivated by SARS-CoV-2 and are prematurely aging, harming organs, and becoming exhausted trying to rid the body of an immune-evasive virus.
If he is right, then no, we cannot assume that T cells will save us — not as thoroughly, at least, as we’ve been led to believe.
What If COVID Reinfections Wear Down Our Immunity?
In a recent study published in the journal Immunity, a team of researchers from the United States found that previous severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections reduce the activation and expansion of CD8+ T cells in response to coronavirus disease 2019 (COVID-19) vaccinations.
SARS-CoV-2 infection damages CD8+ T cell response
We hypothesize that COVID-19 contributed to the 2022 surge of severe pediatric RSV diseases, likely through its damage to the immune and respiratory systems of young children.
Disrupted seasonality and association of COVID-19 with medically attended respiratory syncytial virus infections among young children in the US: January 2010–January 2023
Covid can cause diabetes
a new study from the province of British Columbia in Canada, a comprehensive population assessment, is the 12th report of a heightened risk of Type 2 diabetes after Covid.
New diabetes post-acute Covid (PASC, Long Covid), an inconvenient truth
…
In summary, Type 2 diabetes has been consistently shown to be an adverse outcome in the sub-acute (beyond 30 days) time after a Covid infection. … It’s all the more reason to prevent Covid infections and reinfections.
Long Covid depleting workforces and potentially impacting economies
Just like a cold/mild flu … Not!
//Since the start of the pandemic, cumulatively 2.9 million people of working age (7% of the total) in the UK have had, or still have, Long COVID. This figure will continue to rise due to very high infection rates in the Omicron wave. Since the beginning of the pandemic, economic inactivity due to long-term sickness has risen by 120,900 among the working-age population, fuelling the UK’s current labour shortage. An estimated 80,000 people have left employment due to Long COVID.//
The impact of Long COVID on the UK workforce
A report released by Canada’s chief science adviser says she considers COVID-19 the “head” of the pandemic but long COVID its “tail” as the illness inflicts significant harm on individuals, their families and potentially the country’s economy.
Dr. Mona Nemer said about 10 to 20 per cent of people with COVID-19 develop long COVID after they have recovered from infection and struggle with a variety of symptoms ranging from high blood pressure and an irregular heartbeat to medically undefined symptoms such as chronic fatigue, brain fog, muscle pain and blurred vision.
Report says long COVID could impact economy and be ‘mass disabling event’ in Canada
Vitamin C and l-arginine may help
Worth a try? – I’m taking, after covid, in hope they may be beneficial.
Following a 30-day treatment in both groups, the survey revealed that patients in the L-Arginine + Vitamin C treatment arm had significantly lower scores compared to patients who had received the multivitamin combination.
Combining L-Arginine with vitamin C improves long-COVID symptoms: The LINCOLN Survey
Microbiome may play a role
There is also some evidence Long Covid may be more frequent in people with a poor or disrupted microbiome; here too it is possible to take countermeasures:
Whether you have had COVID-19 or not, the virus is now part of our lives, so it’s a smart idea to make your microbiome as strong as possible, experts say.
“In general, to maintain a healthy microbiome, eat a diverse diet, meaning that you should avoid eating the same things all the time,” said LaBaer. “A diet rich in foods that are not heavily processed, as well as some probiotic foods, will also encourage a more diverse gut microbiome.”
In short: the more diverse your gut bacteria are, the more ground they can cover when it comes to fighting off illness.
COVID Harms Your Microbiome and Long-Term Health: Study